17. Ligation and division
• Approach
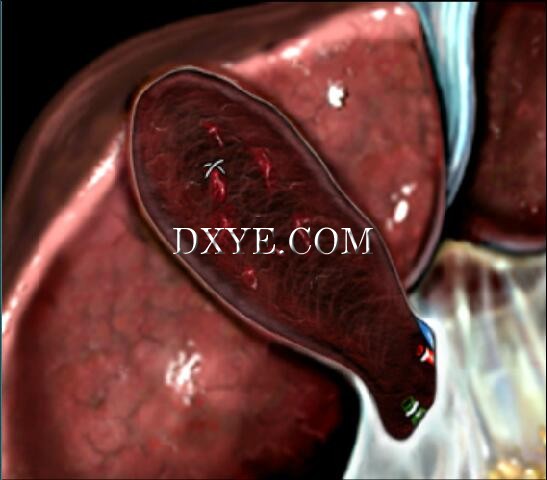
This operative step is delicate and often hemorrhagic due to the inflammation of the tissues. There is sometimes no dissection plane between the liver and gallbladder. Conventionally, a retrograde approach is used to perform the cholecystectomy, but this will depend on the operative findings and difficulties, which may necessitate a change in strategy.
• Division
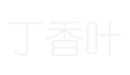
• Cystic artery

The cystic artery may adhere tightly to the gallbladder and hepatoduodenal ligament. It must be meticulously dissected before being clipped and divided.
• Cystic duct
The division of the cystic duct should be performed as close to the gallbladder as possible, checking that no stones are present in the distal portion of the cystic duct.
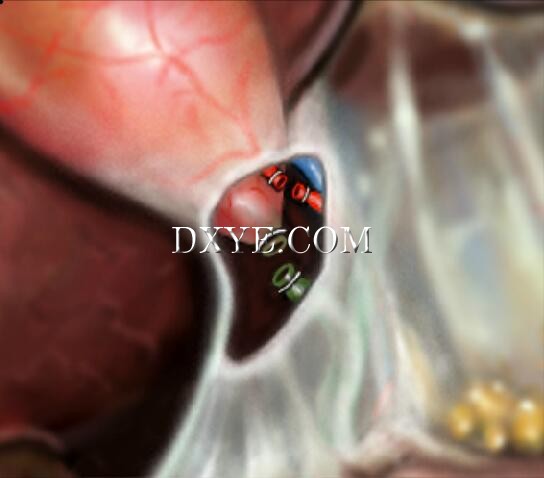
• Retrograde dissection
Dissection of the gallbladder bed can be performed using a hook electrode or scissors. These instruments are useful when dense fibrotic tissues are present between the liver parenchyma and the gallbladder wall. In case of major inflammation, liberation of the gallbladder from the liver may be difficult and hemorrhagic since the plane of cleavage is barely, if not at all, existent. When the plane is difficult to find, part of the gallbladder wall can be left in contact with the liver.
• Hemostasis of gallbladder bed
To achieve hemostasis of the gallbladder bed, in addition to electrocautery, it is sometimes necessary to use an absorbable hemostatic gauze sponge or 'figure of eight' stitches. Certain authors use other methods, such as the Argon Beam.
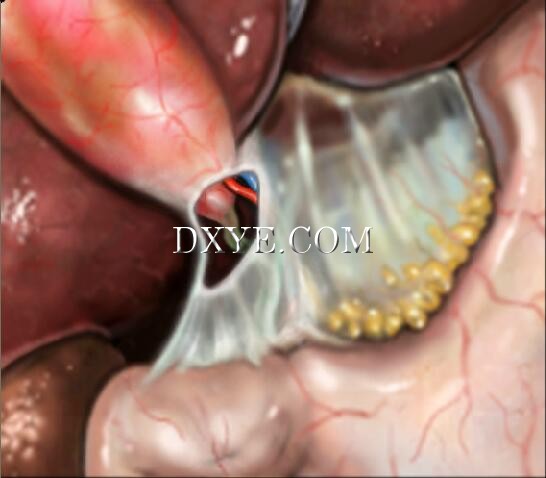
• Danger: enlarged cystic duct
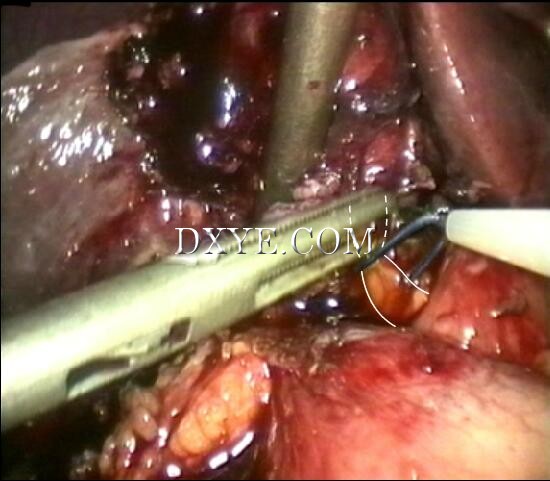
After ligation, the cystic duct is divided at a distance from the CBD.
Putting clips on an inflammatory and often enlarged cystic duct is risky. Clips must therefore be used with caution.
If the outer measurement of the cystic duct is over 6 mm in diameter, it cannot be closed with clips of 8 mm maximal length. In this case we suggest using either a ligature with an intra- or extra-corporeal knot (eg, surgical loop), or placing a suture on the cystic stump.
• Variation: dissection of gallbladder bed
In case of difficulty in identifying the plane of dissection between the gallbladder and the liver (<10% of cases), part of the gallbladder wall can be left in contact with the liver. In this case, the mucosal surface of the gallbladder wall that is embedded in the liver bed is cauterized. |