马上注册,结交更多好友,享用更多功能,让你轻松玩转社区。
您需要 登录 才可以下载或查看,没有账号?注册
×
本帖最后由 小针刀 于 2016-8-29 08:58 编辑
Steinert's disease(斯太纳特病;营养不良性肌强直/Myotonic Dystrophy)-医学百科
强直性肌营养不良由Delege(1890)首先描述。肌强直表现受累的骨骼肌收缩后松弛显著延迟,导致明显的肌肉僵硬,肌电图出现特征性连续高频电位放电现象。
临床表现
本病可发生于任何年龄,但多见于青春期后,男多于女。主要症状为肌无力、肌萎缩和肌强直。萎缩和无力表现为四肢不灵活,前臂及手部肌肉萎缩,下肢有足下垂及跨阈步态。萎缩还可发展至面肌、咬肌、颞肌和胸锁乳突肌,故病人面容瘦长,颧骨隆起,呈斧状脸,颈消瘦而稍前屈。部分病人可有讲话及吞咽困难。肌强直分布不如先天性肌强直那样广泛。
多限于上肢肌肉和舌肌。肌萎缩与肌强直之间并无明显的关系。大部分病人有白内障、多汗、秃发、基础代谢率下降、肺活量减少、消瘦、月经不调、阳痿、性欲下降和不孕等。尚可有胃肠道平滑肌功能障碍,部分病人智力衰退甚至痴呆。
症状体征
强直性肌营养不良症1型(MDI)
通常在30或40岁时显现症状,尽管儿童早期也可出现。男性多于女性,且症状较重。主要症状是肌无力、肌萎缩和肌强直,前两种症状更突出。肌无力见于全身骨骼肌,前臂肌和手肌无力伴肌萎缩和肌强直,有足下垂及跨阈步态,行走困难易跌跤;部分病人构音障碍和吞咽困难。肌萎缩常累及面肌、咬肌、颞肌和胸锁乳突肌,病人面容瘦长,颧骨隆起,呈斧状脸,颈部瘦长稍前驱。肌强直常在肌萎缩前数年或同时发生,分布不如先天性肌强直广泛,仅限于上肢肌、面肌和舌肌。检查可证明肌强直存在,如患者持续握拳后不能立即将手松开,需重复数次后才能放松;用力闭眼后不能立即睁眼,愈咀嚼时不能张口等。用诊锤扣击肌肉的肌呈持续收缩,局部有肌球形成,多见于前臂和手部伸肌,持续数秒后恢复原状,此体征对诊断本病有重要价值。
强直型肌营养不良症2型(MD2)
偶有患者临床表现与强直应肌营养不良症类似,但无肌强直性蛋白激酶基因重复性扩增。临床特征与MD1相似,表现显著的肢体远端肌、面肌、胸锁乳突肌的肌无力和肌萎缩,伴肌强直,也可有白内障、额秃、睾丸萎缩、糖尿病、心脏异常和智力异常等。
近端肌强直性肌病
表现肌强直、近端为主肌无力和白内障,病程不如MD1严重,也曾报道肌肉严重受累并有听力丧失的变异型。
4、许多患者伴白内障、视网膜变性、眼球内陷眼睑下垂、多汗、消瘦、心脏传导阻滞、心律失常和基础代谢率下降等,约半数伴智能低下男性常见睾丸萎缩,但生育力很少下降,因此本病能在家族中传播。玻璃体红晕为早期特征性表现。本病进展缓慢,部分病人因肌萎缩及心、肺等并发症在40岁左右丧失工作能力,常因继发感染和心力衰竭死亡;轻症者病情可长期稳定。
疾病病因
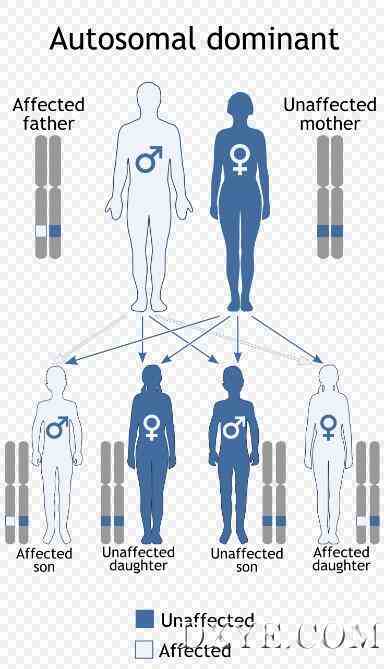
强直性肌营养不良症1型是一种多活动受累的常染色体显性遗传病,基因缺陷位于染色体19q13.2-19q13.3基因三核苷酸(CTG)重复序列扩增,这种扩增的三核苷酸重复构成了诊断试验的基础。这一基因编码的蛋白被称为肌强直性蛋白激酶。基因外显率为100%。全球患病率为3-5/10万,发病率约为1/8000活婴,是成人最常见的肌营养不良症,无明显地理或种族差异。肌强直的发病机制不清,认为是广泛的膜异常,包括骨骼肌膜、红细胞膜、晶状体膜和血管膜等。至少在某些病例,肌纤维膜异常似乎与跨肌纤维膜氯离子电导率降低有关。除表现多组肌群肌萎缩和肌强直外,还有晶状体、皮肤、心脏、内分泌和生殖活动等多活动。强直型肌营养不良症2型的遗传方式不同。一组相关的强直性病变近端肌强直性肌病通常为显性遗传,也有散发病例,与萎缩性肌强直蛋白激酶(DMPK)基因无关,基因定位于3q21.3染色体。
病理生理
典型肌肉病理改变为细胞核内移,呈链状排列,肌细胞大小不一,呈镶嵌分布;肌原纤维往往向一侧退缩形成肌浆,肌细胞坏死和再生不明显。
诊断检查
辅助检查
1、肌电图出现典型肌强直放电,受累肌肉出现连续高频强直波逐渐衰减,肌电图扬声器发出一种类似俯冲轰炸机或链锯样声音;67%的患者运动单位时限缩短,48%有多相波。心电图常可发现传导阻滞及心律失常
2、血清CK和LDH等肌酶滴度或轻度增高。
3、肌活检显示轻度非特异性肌源性损害。
4、基因检测具有特异性,患者染色体19q13.3位点DMPK基因CTG三核苷酸序列异常重复扩增超过100(正常人为5-40),重复数目与症状严重性相关。
诊断及鉴别诊断
1、诊断
根据中青年起病的特征性肌无力、肌萎缩和肌强直症状,主要累及四肢远端肌、头面部肌和胸锁乳突肌;体检可见肌强直,扣击出现肌球,典型肌强直放电肌电图,以及DNA分析出现异常CTG重复扩增等。
2、鉴别诊断
临床需要与其他类型肌强直鉴别
(1)先天性肌强直(congenital myotonia):Thomsen(1876)描述了他本人及其家族的四代患者,又称为Thomsen病。通常为常染色体显性遗传病,与7q35染色体突变有关。通常自出生就存在全身性肌强直,不伴肌无力和肌萎缩,但至儿童早期症状才进展,成年期趋于稳定。肌强直表现与强直性肌肉营养不良相似,寒冷和静止不动肌肉僵硬可加重,活动可缓解。肌肉假肥大是很突出的征象,全身肌肉肥大貌似运动员,扣击肌肉出现局部凹陷或呈肌球症;有时可出现精神症状如易激动、情绪低落、孤僻、抑郁及强迫观念等。肌电图呈典型肌强直电位。一种晚发常染色体隐性遗传型(Becker病)伴远端轻度肌无力和肌萎缩,也定位于7q35染色体。
(2)先天性副肌强直:幼年起病,肌强直较轻,无肌萎缩,肌肥大不明显。
治疗方案
本病无有效的治疗方法,是对症治疗。
①肌强直可用膜系统稳定药治疗,能促进钠泵活动,降低膜内钠离子浓度,提高静息电位,改善肌强直状态;如硫酸奎宁,300-400mg,3次/d;普鲁卡因胺0.5-1g,4次/d;甲妥英0.1g,3次/d;强直性肌营养不良可能首选苯妥英,因其他药物对心脏传导有不良影响;
②肌无力尚无治疗方法,肌萎缩可试用苯丙诺龙治疗,加强蛋白合成代谢;今年里用灵芝制剂有一定的疗效;
③康复疗法对保持肌肉功能有益成年患者应定时检查心电图和眼疾。
安全提示
1、患者禁忌或禁服的药物
(1) 庆大霉素、链霉素、卡那霉素、新霉素、四环素、土霉素、杆菌素、多粘菌素;
(2) 非那根、安定、吗啡、乙醚、普鲁卡因(慎用);
(3) 奎宁、奎尼丁、普鲁卡因酰胺;
(4) 箭毒、琥珀酰胆碱、氯化氨酰胆碱;
(5) 蟾蜍及其中成药丸:六神丸、喉症丸等;
(6) 性味寒凉的中药
2、起居有常。首先要安排好一日生活秩序,按时睡眠,按时起床,不要熬夜,要劳逸给合。
3、避风寒、防感冒,肌无力、肌萎缩等患者抵抗力较差,伤风感冒不仅会促使疾病复发或加重,还会进一步降低机体对疾病的抵抗力。
4、饮食要有节,痿证的病机与脾气亏虚关系密切,故调节饮食更为严重,不能过饥或过饱,在有规律,有节度,同时各种营养要调配恰当,不能偏食。
5、注意适量运动,锻炼身体增强体质,但不能运动过量。病情较重的病人或长期期卧床不起的病人,应给予适当的按摩防止褥疮的产生。
7、在治疗上病人应有良好的心态与康复的信心。鼓励病人和病人本身应该有积极乐观的治疗信心,减少病人的心里负担,避免精神刺激和过度脑力(体力)劳累。
7、注意各种感染,生活保持有规律,饮食方面应多食富含高蛋白的食物如:鸡、鸭、鱼、瘦肉、豆腐、黄豆、鸡蛋、植物蛋白与动物蛋白以及新鲜蔬菜水果,营养搭配对病人来讲非常重要,注意食物的易消化性。
8、忌食食物:生冷、辛辣及过咸食物以及烟酒等刺激。服药期间禁食绿豆。
9、中晚期患者,以高蛋白、高营养、富含能量的半流食和流食为主,并采用少食多餐的方式以维护患者营养及水电解质平衡。
其他信息
强直性肌营养不良症:强直性肌营养不良症(Dystrophy Myotomic,Dm)是人肌营养不良疾病中的一种常染色体显性遗传病,发病率至少为 5/10万。该病具有可变的外显率和表观度,致病基因产物不明,肌肉无力首先出现在脸部、颈部、胸锁乳突肌、手臂肌肉和前胫肌;接着影响到舌咽肌肉而造成讲话不清、吞咽障碍,提眼睑肌造成眼睑下垂,咀嚼肌肉无力,和肩胛部肌肉、股四头肌、前臂肌、尤其手部肌肉和足部肌肉无力,所以常常末端肌肉较会受到侵犯。
除了肌肉无力外,这些病人无疑都伴随着肌肉强直现象(Myotonia)。疾病进展缓慢肌肉无力由远侧端进展至近侧端,肌腱反射消失或降低,有些病人在20-30年后会无法走路,需以轮椅代步。一般而言,初始症状常常不明显,等到严重时已经过20-30年,故此病常好发于30岁以后。
此外一些病人如果发病较晚者,常常无肌肉症状而仅有白内障现象。
维基百科:
Myotonic dystrophy (dystrophia myotonica, myotonia atrophica) is a chronic, slowly progressing, highly variable, inherited multisystemic disease. It is an autosomal-dominant disease. It is characterized by wasting of the muscles (muscular dystrophy), cataracts, heart conduction defects, endocrine changes, and myotonia.[1]
There are two main types of myotonic dystrophy. Myotonic dystrophy type 1 (DM1), also called Steinert disease, has a severe congenital form and an adult-onset form. Myotonic dystrophy type 2 (DM2), also called proximal myotonic myopathy (PROMM) is rarer than DM1 and generally manifests with milder signs and symptoms. Myotonic dystrophy can occur in people of any age. Both forms of the disease display an autosomal-dominant pattern of inheritance. Both "DM1" and "DM2" have adult-onset forms.
40岁与双边白内障和完整的心脏传导阻滞肌强直性营养不良表现

Myotonic dystrophy subtypes强直性肌营养不良症的亚型
Type Gene Repeat Anticipation Severity
DM1 DMPK CTG Yes Moderate-severe
DM2 ZNF9 CCTG Minimal/none Mild-moderate
There are two main types of myotonic dystrophy. Type 1 (DM1), also known as Steinert disease, has a severe congenital form and a milder childhood-onset form as well as an adult-onset form [[2]] . This disease in more often in the facial muscles, levator palpebrae superioris, temporalis, sternocleidomastoids, distal muscles of the forearm, hand intrinsic muscles, and ankle dorsiflexors.[3] Type 2 (DM2), also known as proximal myotonic myopathy (PROMM), is rarer and generally manifests with milder signs and symptoms than DM1.[citation needed]
Other forms of myotonic dystrophy not associated with DM1 or DM2 genetic mutations have been described.[4] One case which was proposed as a candidate for the "DM3" label,[5] was later characterized as an unusual form of inclusion body myopathy associated with Paget's disease and frontotemporal dementia.[4][6][7]
Myotonic dystrophy (DM) is an inherited disease, affecting males and females approximately equally. About 30,000 people in the United States are affected. Symptoms may appear at any time from infancy to adulthood. DM causes general weakness, usually beginning in the muscles of the hands, feet, neck, or face. It slowly progresses to involve other muscle groups, including the heart. DM affects a wide variety of other organ systems as well. A severe form of DM, congenital myotonic dystrophy, may appear in newborns of mothers who have DM. Congenital Myotonic Dystrophy can also be inherited via the paternal gene, although it is said to be relatively rare. Many professionals still state it is only via the maternal gene, however this has been disproved in recent years. Congenital means that the condition is present from birth. The incidence of congenital myotonic dystrophy is thought to be about 1:20,000. DM occurs in about 1 per 7,000–8,000 people and has been described in people from all over the world.[citation needed]
Signs and symptoms 体征和症状
Presentation of symptoms and signs varies considerably by form (DM1/DM2), severity and even unusual DM2 phenotypes. DM1 symptoms for DM2 include problems with executive function (e.g., organization, concentration, word-finding) and hypersomnia. Conduction abnormalities are more common in DM1 than DM2, but all people are advised to have an annual ECG. Both types are also associated with insulin resistance. Myotonic dystrophy may have a cortical cataract with a blue dot appearance, or a posterior subcapsular cataract.[8]
DM2 is generally milder than DM1, with generally fewer DM2 people requiring assistive devices than DM1 people.[citation needed] In addition, the severe congenital form that affects babies in DM1 has not been found in DM2 and the early onset of symptoms is rarely noted to appear in younger people in the medical literature. Death from the disease is unlikely but possible in both forms of myotonic dystrophy.[citation needed]
Genetics
遗传学
Myotonic dystrophy is inherited in an autosomal dominant pattern.
Myotonic dystrophy is a genetic condition which is inherited in an autosomal dominant pattern and thus will be passed along to 50% of a carrier's offspring, on average.Myotonic dystrophy is one of several known trinucleotide repeat disorders. Certain areas of DNA have repeated sequences of two or three nucleotides.[citation needed]
DM1
In DM1, the affected gene is called DMPK, which codes for myotonic dystrophy protein kinase,[9] a protein expressed predominantly in skeletal muscle.[10] The gene is located on the long arm of chromosome 19.[11][12]
Histopathology of DM2. Muscle biopsy showing mild myopathic changes and grouping of atrophic fast fibres (type 2, highlighted). Immunohistochemical staining for type-1 ("slow") myosin
In DM1, there is an expansion of the cytosine-thymine-guanine (CTG) triplet repeat in the DMPK gene. Between 5 and 37 repeats is considered normal, while individuals with between 38 and 49 repeats are considered to have a pre-mutation and are at risk of having children with further expanded repeats and, therefore, symptomatic disease.[4] Individuals with greater than 50 repeats are almost invariably symptomatic, with some noted exceptions.[ref] Longer repeats are usually associated with earlier onset and more severe disease.[citation needed]
DMPK alleles with greater than 37 repeats are unstable and additional trinucleotide repeats may be inserted during cell division in mitosis and meiosis. Consequently, the children of individuals with premutations or mutations inherit DMPK alleles which are longer than their parents and therefore are more likely to be affected or display an earlier onset and greater severity of the condition, a phenomenon known as anticipation. Interestingly, paternal transmission of the condition is very uncommon, possibly due to selection pressures against sperm with expanded repeats, but anticipation tends to be less severe than in cases of maternal inheritance.
The RNA from the expanded trinucleotide repeat region forms intranucleoplasmic hairpin loops due to the extensive hydrogen bonding between C-G base pairs, and it has been demonstrated that these sequester the splicing regulator MBNL1 to form distinctive foci by labelling it with GFP and a probe oligonucleotide with the red-fluorescent dye Cyanine5 (Cy5)[13]
强直性肌营养不良是一种常染色体显性遗传模式。
DM2
DM2 is caused by a defect of the ZNF9 gene on chromosome 3.[14] The specific defect is a repeat of the cytosine-cytosine-thymine-guanosine (CCTG) tetranucleotide in the ZNF9 gene.[14] As it involves the repeat of four nucleotides, it is not a trinucleotide repeat disorder, but rather a tetranucleotide repeat disorder.[6][15]
The repeat expansion for DM2 is much larger than for DM1, ranging from 75 to over 11,000 repeats.[14] Unlike in DM1, the size of the repeated DNA expansion in DM2 does not appear to make a difference in the age of onset or disease severity.[4] Anticipation appears to be less significant in DM2 and most current reviews only report mild anticipation as a feature of DM2.
Diagnosis
诊断
This section needs more medical references for verification or relies too heavily on primary sources. Please review the contents of the section and add the appropriate references if you can. Unsourced or poorly sourced material may be challenged and removed. (April 2016)
Rod of Asclepius2.svg
The diagnosis of DM1 and DM2 can be difficult due to the large number of neuromuscular disorders, most of which are very rare. More than 40 neuromuscular disorders exist with close to 100 variants.[citation needed]
As a result, people with multiple symptoms that may be explained by a complex disorder such as DM1 or DM2 will generally be referred by their primary care physician to a neurologist for diagnosis. Depending on the presentation of symptoms, people may be referred to a number of medical specialists including cardiologists, ophthalmologists, endocrinologists, and rheumatologists. In addition, the clinical presentation is obscured by the degree of severity or the presence of unusual phenotypes.
The clinical presentation for both people with DM1 and DM2 commonly differs from the conception of the diseases held by many neurologists. Clinicians who are less familiar with the myotonic dystrophies may expect people with both forms to present with the more severe, classic symptoms of DM1. As a result, people may remain undiagnosed or be misdiagnosed. A useful clinical clue for diagnosis is the failure of spontaneous release of the hands following strong handshakes due to myotonia (delayed relaxation of muscles after contraction) which accompanies muscle weakness.
Though there is presently no cure for DM and management is currently symptom based, a precise diagnosis is still necessary to anticipate multiple other problems that may develop over time (e.g. cataracts). An accurate diagnosis is important to assist with appropriate medical monitoring and management of symptoms. In addition, genetic counseling should be made available to all people because of the high risk of transmission. Potentially serious anesthetic risks are important to note, so the presence of this disorder should be brought to the attention of all medical providers.
Prenatal testing 产前检查
Genetic tests, including prenatal testing, are available for both confirmed forms. Molecular testing is considered the gold standard of diagnosis.
Testing at pregnancy to determine whether an unborn child is affected is possible if genetic testing in a family has identified a DMPK mutation. This can be done at 10–12 weeks gestation by a procedure called chorionic villus sampling (CVS) that involves removing a tiny piece of the placenta and analyzing DNA from its cells. It can also be done by amniocentesis after 14 weeks gestation by removing a small amount of the amniotic fluid surrounding the baby and analyzing the cells in the fluid. Each of these procedures has a small risk of miscarriage associated with it and those who are interested in learning more should check with their doctor or genetic counselor. There is also another procedure called preimplantation diagnosis that allows a couple to have a child that is unaffected with the genetic condition in their family. This procedure is experimental and not widely available. Those interested in learning more about this procedure should check with their doctor or genetic counselor.
Predictive testing 预测性测试
It is possible to test someone who is at risk for developing DM1 before they are showing symptoms to see whether they inherited an expanded trinucleotide repeat. This is called predictive testing. Predictive testing cannot determine the age of onset that someone will begin to have symptoms, or the course of the disease. If the child is not having symptoms, the testing is not possible with an exception of emancipated minors as a policy.
Management 管理
There is currently no cure for or treatment specific to myotonic dystrophy. Therefore, the focus is on managing the complications of the disease, particularly those relating to the cardiopulmonary system as these account for 70% of deaths due to DM1.[4] Pacemaker insertion may be required for individuals with cardiac conduction abnormalities. Improving the quality of life which can be measured using specific questionnaires[16] is also a main objective of the medical care. Central sleep apnoea or obstructive sleep apnoea may cause excessive daytime sleepiness, and these individuals should undergo a sleep study. Non-invasive ventilation may be offered if there is an abnormality. Otherwise, there is evidence for the use of modafinil as a central nervous system stimulant, although a Cochrane review has described the evidence thus far as inconclusive.
Some small studies have suggested that imipramine, clomipramine and taurine may be useful in the treatment of myotonia.[4] However, due to the weak evidence and potential side effects such as cardiac arrhythmias, these treatments are rarely used. A recent study in December 2015 showed that a common FDA approved antibiotic, Erythromycin reduced myotonia in mice.[17] Human studies are planned for erythromycin. Erythromycin has been used successfully in patients with gastric issues.[18]
Altered splicing of the muscle-specific chloride channel 1 (ClC-1) has been shown to cause the myotonic phenotype of DM1 and is reversible in mouse models using Morpholino antisense to modify splicing of ClC-1 mRNA.[19]
Physical activity 体力活动
Combined strengthening and aerobic training at moderate intensity was deemed safe for individuals with neuromuscular diseases[20][needs update] and the combination was found to increase muscle strength.[21] Specifically, aerobic exercise via stationary bicycle with an ergometer was found to be safe and effective in improving fitness in people with DM1.[22] The strength training or aerobic exercise may promote muscle and cardiorespiratory function, while preventing further disuse atrophy.[20] Cardiovascular impairments and myotonic sensitivities to exercise and temperature necessitate close monitoring of people and educating people in self-monitoring during exercise via the Borg scale, heart rate monitors, and other physical exertion measurements.[23]
Orthotics 矫形
Muscular weakness of dorsiflexors (dorsiflexion) hinders the ability to clear the floor during the swing phase of gait and people may adopt a steppage gait pattern[23] or ankle-foot-orthotics may be indicated.[4] Factors such as hand function, skin integrity, and comfort must be assessed prior to prescription. Neck braces can also be prescribed for neck muscle weakness.[4]
Mobility aids and adaptive equipment 助行器和自适应设备
Upper and lower limb weakness, visual impairments and myotonia may lead to the need for mobility aids and functional adaptive equipment such as buttonhooks and handled sponges for optimal hand function. If assistive devices and home adaptations are needed, physical therapists may refer on to occupational therapist(s) for further assessment.[4]
Epidemiology 流行病学
DM1 is the most common form of myotonic muscular dystrophy diagnosed in children, with a prevalence ranging from 1 per 100,000 in Japan to 3-15 per 100,000 in Europe.[4] The prevalence may be as high as 1 in 500 in regions such as Quebec, possibly due to the founder effect. In most populations, DM1 appears to be more common than DM2. However, recent studies suggest that type 2 may be as common as type 1 among people in Germany and Finland.[1]
Research 研究
The years since the discovery of the genetic cause of MMD in 1992 have been fruitful ones for MMD research. Scientists are gaining understanding of how the expanded DNA section on chromosome 19 causes so many physiologic changes. In the meantime, scientists are also working to test drug treatments that may help symptoms in MMD. Among these are a drug that can make muscles more sensitive to insulin, one that may help improve muscle function and one that may relieve myotonia. The ultimate cure for MMD would probably require finding a way to block the expanded area of DNA on chromosome 19 or chromosome 3 so that it would lose its toxic effect on cells. It is not far-fetched to imagine that, in the future, this expanded section of DNA could be blocked or silenced. Scientists around the world are studying the unusual biological mechanisms that underlie MMD and working on pathways to treatment. However, it needs to be understood that such a treatment will take many years to be sufficiently developed to be used on humans. Ionis Pharmaceutical along with Biogen is currently in Phase 1/2 clinical trials to test an antisense compound to treat Myotonic Dystrophy type 1.[citation needed]
|